How Long Do Dental Implants Last on Average?
Dental implants are often hailed as the gold standard for tooth replacement, but if you’re considering getting one, you probably have one big question in mind:
“How long do dental implants actually last?”
It’s a fair concern—after all, implants require surgery, time, and a financial investment. In this blog, we’ll break down the average lifespan of dental implants, what affects their longevity, and how you can make yours last a lifetime.
The Short Answer: 10+ Years or Even a Lifetime
On average, dental implants can last 10 years or more, and in many cases, they last a lifetime.
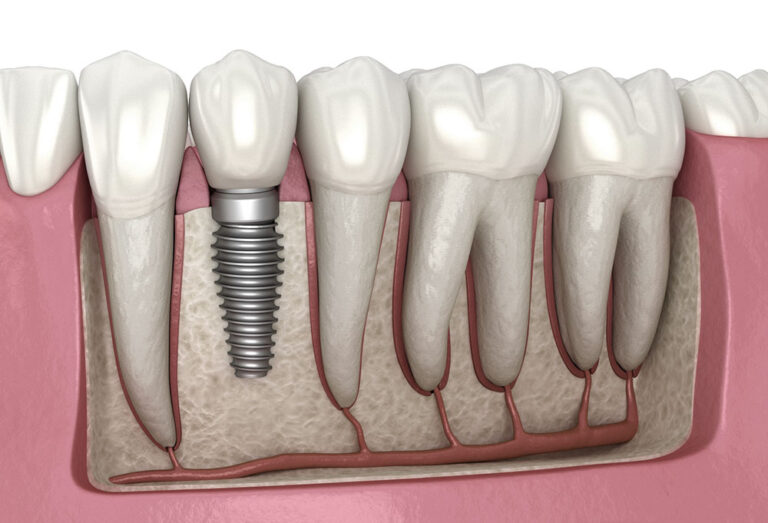
A dental implant consists of three main parts:
- The Implant Post (Titanium/Zirconia Root) – This is surgically placed into the jawbone and is designed to last permanently.
- The Abutment – A connector that attaches the crown to the implant.
- The Crown (Artificial Tooth) – This is the visible part that may need replacement after 10–15 years due to wear and tear.
So, while the implant post is built to last a lifetime, the crown might need occasional maintenance or replacement over the years.
What Affects the Lifespan of a Dental Implant?
Not all implants last the same amount of time. Here’s what determines how long yours will stay strong:
1. Oral Hygiene Habits
Maintaining excellent oral hygiene is one of the most important factors in ensuring the longevity of a dental implant. Although implants themselves do not develop cavities, the surrounding gum tissue and bone require constant care to prevent infections. One of the biggest risks is peri-implantitis, a bacterial infection that causes inflammation around the implant. If left untreated, peri-implantitis can lead to bone loss and ultimately implant failure.
To protect your implant, establish a rigorous oral hygiene routine. Brush your teeth at least twice a day using a soft-bristled toothbrush and non-abrasive toothpaste to prevent damage to the implant crown. Floss daily, using special floss or interdental brushes designed for implants, to remove plaque and food particles from hard-to-reach areas. Additionally, incorporating an antibacterial mouthwash can help control bacteria levels and reduce the risk of infection. Regular dental check-ups and professional cleanings are essential for monitoring the health of your implant and catching potential issues early.
2. Smoking
Smoking is one of the most significant risk factors for dental implant failure. Nicotine and other harmful chemicals in tobacco products reduce blood flow to the gums, impairing the body’s ability to heal properly after implant surgery. This diminished circulation slows down osseointegration, the process by which the implant fuses with the jawbone, increasing the risk of early implant failure.
Additionally, long-term smoking contributes to gum recession and bone loss, two critical factors that can lead to peri-implantitis, an infection that causes inflammation and deterioration of the bone surrounding the implant. Studies indicate that implant failure rates are nearly double in smokers compared to non-smokers. Furthermore, smoking weakens the immune system, making it harder for the body to fight off infections that could compromise the stability of the implant over time.
If you are a smoker considering dental implants, reducing or quitting smoking before and after surgery can significantly increase your chances of long-term implant success. Your dentist may recommend smoking cessation programs or alternative strategies to help improve healing and ensure your implant lasts as long as possible.
3. Teeth Grinding (Bruxism)
Bruxism, or teeth grinding, is a common yet often overlooked factor that can significantly impact the longevity of dental implants. Many individuals grind their teeth unconsciously, especially at night, exerting excessive pressure on the implant and surrounding bone. This continuous force can cause micro-movements in the implant, preventing proper osseointegration and potentially leading to implant loosening or failure over time.
Chronic bruxism can also wear down the implant-supported crown faster than normal, leading to premature replacement. Additionally, excessive grinding places strain on the jaw muscles and temporomandibular joints (TMJ), which can result in discomfort or complications in bite alignment.
To protect your dental implant, it is essential to identify and manage bruxism early. A custom-made nightguard, designed specifically for individuals with implants, can help absorb the force of grinding and protect both natural teeth and implants from excessive stress. Stress management techniques, lifestyle modifications, and regular dental visits can also help monitor and address the effects of bruxism before they become severe.
4. Overall Health and Bone Quality
Your overall health plays a crucial role in determining how well a dental implant integrates with your jawbone and how long it will last. Conditions such as osteoporosis, diabetes, and periodontal (gum) disease can negatively impact bone density and healing, making it more challenging for an implant to remain stable over time.
Osteoporosis, a condition that weakens bones, can reduce the jawbone’s ability to support an implant, increasing the risk of implant failure. Diabetes, particularly if uncontrolled, can slow down healing after implant surgery and increase the likelihood of infections, which may lead to peri-implantitis. Gum disease, if left untreated, can cause inflammation and bone loss around the implant, ultimately leading to failure.
To ensure the longevity of a dental implant, it is essential to manage these health conditions effectively. If you have osteoporosis, your dentist may recommend bone-strengthening treatments or a thorough evaluation of your bone density before proceeding with an implant. For diabetics, maintaining stable blood sugar levels through diet, medication, and lifestyle choices can significantly improve healing and reduce infection risks. If you have a history of gum disease, regular periodontal care, including deep cleanings and professional check-ups, is essential to prevent complications.
Before undergoing implant surgery, discuss your medical history with your dentist. A collaborative approach between your dentist and primary healthcare provider can help optimize your overall health, increasing the chances of long-term implant success.
How Can You Make Your Implants Last a Lifetime?
The good news is that most implant failures are preventable with proper care. Here are five simple steps to ensure yours lasts as long as possible:
- Practice good oral hygiene – Brush, floss, and use an antibacterial mouthwash.
- Visit your dentist regularly – Routine check-ups can catch problems early.
- Avoid smoking and excessive alcohol – Both can weaken your bones and gums.
- Wear a nightguard if you grind your teeth – Protect your implant from unnecessary pressure.
- Eat a healthy diet – Nutrients like calcium and vitamin D support strong bones and gums.
Final Thoughts: Are Implants Worth It?
Absolutely. With proper care, dental implants can last a lifetime, making them a fantastic long-term investment in your smile, confidence, and oral health.
If you’re considering an implant and have concerns about longevity, talk to your dentist to ensure you’re a good candidate. And if you already have implants, treat them like natural teeth, and they will serve you well for decades to come.
References
Misch, C. E. (2020). Contemporary Implant Dentistry (4th ed.). Elsevier.
Lang, N. P., & Berglundh, T. (2011). Peri-implant diseases: where are we now? – Consensus of the Seventh European Workshop on Periodontology. Journal of Clinical Periodontology, 38(s11), 178-181.